The Larynx: Structure and Function
Most singers and speakers are aware of the existence of the larynx, colloquially known as the 'voice box', but understand very little about its structure and function, and the role of the vocal folds, (formerly called 'vocal cords'), in voice production and in the creation of pitch. While I don't believe that it is necessary for a singer to memorize all the parts and functions of the individual structures within the throat - we can leave that for the medical students - I do believe that gaining a better understanding of how the larynx works and what the vocal folds are and do can help a student of voice achieve technical proficiency and maintain vocal health.
My intention in this section is to provide some basic information about the highly complex structure of the larynx, and how the primary structures of the larynx affect vocal function. I'll attempt to make descriptions and explanations as succinct and as clear as possible, and focus only on the principle cartilages, joints, bones, ligaments and muscles that help to produce the voice. However, given that the parts that make up the larynx are intricate and function in unique ways, and given that scientific and/or medical terms are sometimes the best ones (or the only ones) to use when discussing human anatomy, it may be impossible to truly simplify everything as much as I would like to. My suggestion is that singers thoroughly read the following sections and attempt to understand and learn whatever they can. Again, what is most important is that the student of voice gains a glimpse into the fascinating and complex - far more complex than any other instrument - structure that produces the voice and comes to develop a better appreciation for his or her built-in instrument.
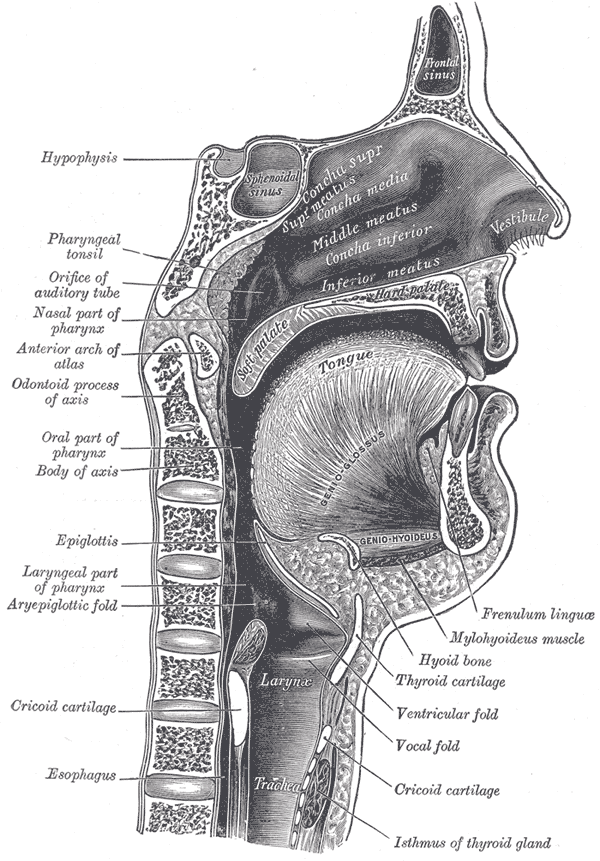
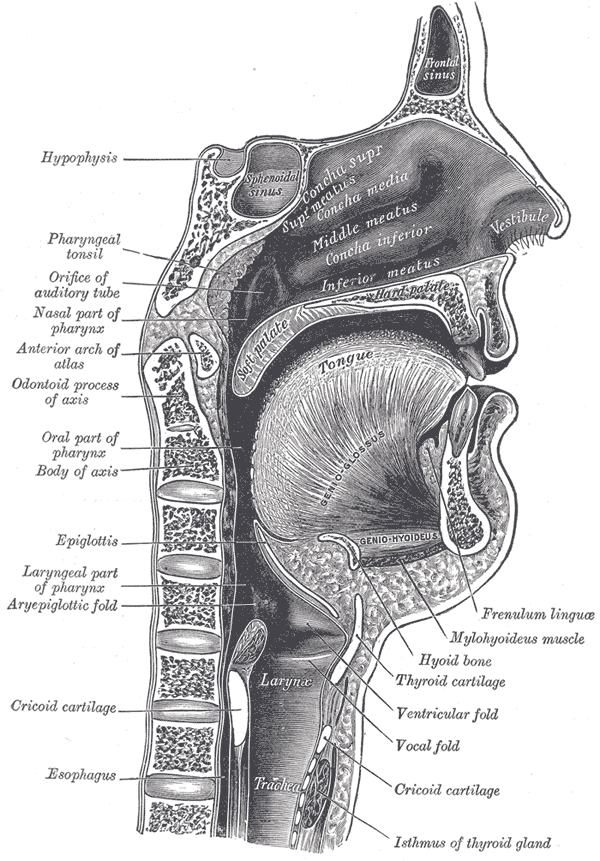
ANATOMY OF THE VOCAL TRACT
Dorland's Medical Dictionary for Health Consumers. - 2007 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
POSTERIOR VIEW OF ANTERIOR WALL OF LARYNX
The vocal folds, together with the muscles and cartilages that support them, are known as the larynx.
The larynx is an organ in the neck that lies in front of the fourth, fifth, and sixth cervical vertebrae. It is situated just below where the tract of the pharynx (the part of the neck and throat situated immediately behind the mouth and nasal cavity, and above the esophagus, larynx, and trachea) splits into the trachea (the 'windpipe' or tube that allows the passage of air into the lungs) and the esophagus (a muscular tube through which food passes from the pharynx to the stomach). The larynx is involved in both the protection of the trachea and in the production of sound.
The upper entrance of the larynx - that which is continuous with pharynx - is a triangular opening that is narrow in front and wide behind, and slants downward and backward. The lower portion is continuous with the trachea and is circular. It is bordered in front by the epiglottis behind, by the arytenoid cartilages, the corniculate cartilages, and the interarytenoid notch (the indentation of the posterior portion of the aditus laryngeal inlet between the two arytenoid cartilages); and on either side, by the aryepiglottic fold, on the posterior part of the margin of which the cuneiform cartilages form a whitish prominence called the cuneiform tubercle. These folds form the upper borders of the quadrangular membrane.
SPACES OF THE LARYNX
from http://www.yorku.ca/earmstro/journey/larynx2.html
This image here shows the spaces created by the various structures of the larynx.
The first space in the larynx is called the vestibule, which is the space above the vestibular fold (false vocal fold). Just beneath the vestibular fold is the ventricle (not shown), which extends laterally and is connected anteriorly to a small sac called the saccule (also not shown). The saccule has special cells that produce a secretion to keep the vocal folds moist. Beneath the ventricle is the true vocal fold that extends from the vocal process of the arytenoid cartilages to the backside of the thyroid cartilage.
The larynx is connected with the pharynx by the opening or thin space between the right and left vocal folds and the arytenoid cartilages, called the glottis (or rima glottidis or rima glottides), through which air must pass in order to vocalize and breathe. The part between the arytenoid cartilages is called the intercartilaginous part (or the intercartilaginous glottis, respiratory glottis, or interarytenoid space), and the part between the vocal folds is called the intermembranous part (or glottis vocalis). The rima glottidis is closed by the lateral cricoarytenoid and arytenoid muscles, and its entrance is protected by the epiglottis.
The area below the glottis is called the infraglottic cavity (or infraglottic space). Below the infraglottic cavity is the trachea ('windpipe').
The larynx consists of four basic anatomic components: a cartilaginous skeleton, intrinsic muscles, extrinsic muscles, and a mucosal lining.
SKELETON OF THE LARYNX
from http://home.comcast.net/~wnor/lesson11.htm
SKELETON OF THE LARYNX (ANTEROLATERAL VIEW)
from http://home.comcast.net/~wnor/lesson11.htm
SKELETON OF THE LARYNX (POSTERIOR VIEW)
The skeleton of the larynx is made up of the hyoid bone and several cartilages. There are nine cartilages of the larynx, three of which (the thyroid, the cricoid and the epiglottis) are unpaired, and three of which (the arytenoids, the corniculates, and the cuneiforms) are paired. These cartilages support the larynx and form its skeleton. They are connected to other structures of the head and neck through the extrinsic muscles. (The intrinsic muscles of the larynx alter the position, shape and tension of the vocal folds.)
The hyoid bone is a horseshoe-shaped (or U-shaped) bone situated in the anterior midline of the neck between the chin and the thyroid cartilage. At rest, it lies at the level of the base of the mandible (lower jaw) in the front and the third cervical vertebra behind. It is the only bone in the human skeleton that does not make contact with, or connect to, any other bone. The hyoid bone is not technically part of the larynx, though it is connected to it - to the thyroid cartilage - by the thyrohyoid membrane, and is held in place by the thyroid ligaments. The hyoid bone provides attachment to the muscles of the floor of the mouth and the tongue above, the larynx below, and the epiglottis and pharynx behind. It allows a wider range of tongue, pharyngeal and laryngeal movements by bracing these structures alongside each other in order to produce variation. During swallowing, the hyoid bone elevates, (also pulling the larynx upward with it), in order to guard the entrance of the airway against the introduction of food and other swallowed matter.
The cartilaginous skeleton refers to the cartilage structure in and around the trachea that contains the larynx, or houses the vocal folds, (which used to be called the 'vocal cords'). It is comprised of the thyroid, cricoid, and arytenoid cartilages.
The thyroid cartilage is the largest of the nine cartilages that make up the laryngeal skeleton. It is attached to the hyoid bone and is made up of two plate-like laminae (thin cartilages) that fuse on the anterior (front) side of the cartilage to form a peak, lump or protrusion called the laryngeal prominence, (otherwise known as the Adam's apple). The angle of the thyroid cartilage surrounding the larynx is usually more acute in adult males - the two laminae of the thyroid cartilage that form the protrusion meet at an average of 90�in males, as opposed to 120�in females - and is therefore more pronounced. The thyroid cartilage forms the bulk of the anterior wall of the larynx, making up the body of the larynx, and serves to protect the vocal folds, which are located directly behind it. It also serves as an attachment for several laryngeal muscles.
The lip of the thyroid cartilage just superior to the laryngeal prominence is called the superior thyroid notch, while the notch inferior to the thyroid angle is called the inferior thyroid notch. Its posterior border is elongated both inferiorly and superiorly to form the superior horn of thyroid cartilage and inferior horn of thyroid cartilage. The inferior horns articulate with (connect with or come in contact with) the sides of the cricoid cartilage - see next paragraph - and form the cricothyroid joint, where the thyroid cartilage rocks back and forth, or pivots, at this point.
The cricoid cartilage is the only complete cartilaginous ring of the larynx and is the strongest of all the laryngeal cartilages. It is made of hyaline cartilage, (consisting of a slimy mass of a firm consistency, but of considerable elasticity and pearly bluish color), and can become calcified or even ossified, particularly in old age. It is shaped like a signet ring with a broad arch (the cricoid arch) on its posterior side - where it forms a square-shaped lamina (the cricoid lamina). As it extends upward to form the posterior border of the larynx, it tapers anteriorly to a narrow arch. Its anterior part is called the band. The cricoid is attached to the top of trachea, to the first tracheal ring, by the cricotracheal ligament. The cricoid cartilage provides attachments for the various muscles, cartilages, and ligaments involved in opening and closing the airway and in speech production.
The epiglottis is a large, leaf-shaped flap of elastic cartilage tissue that is attached to the root of the tongue and inferiorly to the thyroid cartilage by a small stem. During breathing, the epiglottis is pointed upward to allow air to freely enter and exit the trachea and lungs. During swallowing, however, the backward motion of the tongue forces the epiglottis over the laryngeal opening - it folds down into a horizontal position like a lid - to prevent swallowed material from entering the larynx and lungs, which would produce irritation and a strong cough reflex. The larynx is also pulled upwards with the elevation of the hyoid bone to assist this process.
The arytenoid cartilages are triangular (or pyramidal) pieces of mostly hyaline cartilage that sit on top of the cricoid lamina, posteriorly, and articulate there at the cricoarytenoid joints. The arytenoid cartilages slide and rotate on an axis at these joints. The movements that take place between the arytenoid and cricoid cartilages - that is, at the cricoarytenoid joints - include adduction (drawing together), abduction (pulling apart), anterior-posterior sliding, and medial-lateral sliding.
The triangular base of the arytenoid cartilages contains three processes: the vocal process, the muscular process, and a third process that is not well defined. The anterior angle of the base of the arytenoid cartilage - the medial process - is called the vocal process. It projects horizontally forward and gives attachment to the vocal ligament (vocal fold), which extends from the vocal process to the backside of the thyroid cartilage. Of the paired cartilages, the arytenoid cartilages are the most important because they influence the position and tension of the vocal folds. Any movement of the arytenoid cartilage will have an effect on the vocal folds (e.g., making them loose or taut, bringing them together or spreading them apart). The muscular process of the arytenoids - the lateral process - lies laterally, and most of the muscles that act to abduct (open) or adduct (close) the vocal folds attach to it. The arytenoid cartilages are pulled towards each other (approximated) by the transverse arytenoid muscle.
The paired corniculate cartilages are two small conical (or horn-shaped) nodules consisting of pieces of hyaline (yellow elastic) cartilage that articulate with the apex (summits) of each arytenoid cartilage, and serve to prolong them posteriorly and medially. They are situated in the posterior parts of the aryepiglottic fold, and are sometimes fused with the arytenoid cartilages.
The paired cuneiform cartilages are small, elongated, club-shaped pieces of yellow elastic cartilage located anterior to the corniculate cartilages. On the posterior part of the margin of the aryepiglottic fold, just in front of the arytenoid cartilages, they form a whitish prominence on the surface of the mucous membrane called the cuneiform tubercle.
INTRINSIC MUSCLES OF THE LARYNX
The muscles of the larynx consist mainly of muscles that change the opening of the glottis, as well as the tenseness of the vocal folds, thereby keeping the glottis open during respiration or more closed during vocalization. The extrinsic muscles connect the thyroid, cricoid, and arytenoid cartilages to other structures of the head and neck, while the smaller muscles within the structure of the larynx, the intrinsic muscles, move the vocal folds in reference to each other. The intrinsic muscles of the larynx abduct (move apart), adduct (bring together), alter vocal fold shape or change the longitudinal tension of the folds.
The cricothyroid muscle lengthens and stretches the vocal folds. It lies anterior and external to the larynx, and is part of the muscular triangle of the neck. It arises from the cricoid cartilage and attaches to the inferior horn and lower margin of the thyroid cartilage. When it contracts, it pulls the thyroid cartilage forward around the axis through the cricothyroid joint, increasing the distance between the thyroid and arytenoid cartilages and stretching and tensing the vocal fold. (The action of the cricothyroid tilts the thyroid cartilage down, increasing the front-to-back distance of the larynx, and thus placing the vocal folds under increased tension. This action is often referred to as the 'laryngeal tilt' or 'rocking/pivoting the larynx', and is important in being able to sing higher pitches.) Unlike all the other muscles of the larynx, which are innervated by the recurrent laryngeal nerve (branch) of the vagus, the cricothyroid muscle is the only muscle that is supplied by the external laryngeal branch of the vagus (superior laryngeal nerve).
The cricothyroid ligament is the larger part of the laryngeal membrane, continuing inferiorly as a median or anterior part and twin lateral ligaments. The median cricothyroid ligament is a flat band of white tissue joining the cricoid and thyroid cartilages, while the lateral cricothyroid ligament (also known as the cricothyroid membrane) keeps the cricoid and thyroid from traveling too far.
The lateral cricoarytenoid muscle arises from the upper border of the cricoid cartilage and inserts into the muscular process of the arytenoid cartilages. The lateral cricoarytenoid muscles adduct and internally rotate the arytenoid cartilages to close the rima glottides (glottis).
The posterior cricoarytenoid muscles arise from the expanse of the cricoid lamina and insert into the muscular process of the arytenoid cartilages. These muscles adduct and externally or laterally rotate the arytenoid cartilages, causing the vocal folds to separate from one another, thus opening the rima glottidis. These are the only muscles that are capable of opening the space between (abducting) the vocal folds to allow for normal breathing. If this muscle is incapacitated on both sides, as in a bilateral injury to the recurrent laryngeal nerve, the inability to pull the vocal folds apart will cause difficulty in breathing.
The transverse arytenoid muscle is a single muscle that arises from the posterior surface and lateral border of one arytenoid cartilage and is inserted into the corresponding parts of the opposite (arytenoid) cartilage, and fills up the posterior concave surfaces of the arytenoid cartilages. The transverse arytenoid muscle pulls the arytenoids toward each other when they contract, which results in adducted vocal folds. This action closes the rima glottides (the opening of the glottis), especially at its back part, to eliminate the posterior commissure - the point, angle, or surface where two parts join or connect - of the vocal folds.
The aryepiglottic fold (or aryepiglottis) is a fold of mucous membrane, enclosing ligamentous and muscular fibres, that extends from the side of the epiglottis to the apex of the arytenoid cartilage, forming the borders of the opening of the larynx.
Located in the upper part of the aryepiglottic fold is the aryepiglottic muscle (aryepiglotticus or recurrent laryngeal nerve of the vagus). It is attached to the lateral border of the epiglottis and becomes the oblique arytenoid muscle, which then attaches into the arytenoid cartilage. This muscle works as a sort of purse string to close the opening of the larynx when swallowing, protecting the larynx. The oblique arytenoids narrow the laryngeal inlet by constricting the distance between the arytenoid cartilages and the epiglottis. (When the aryepiglottis contracts, it causes the arytenoids to appose each other - it closes the laryngeal aditus by bringing the aryepiglottic folds together - and draws the epiglottis down to bring its lower half into contact with the arytenoids, thus closing the aditus.)
The thyroarytenoid muscle is a broad, thin muscle that lies parallel with and lateral to the vocal fold and extends from the lower half of the back of the thyroid cartilage to the front side of the arytenoid cartilage, to the middle cricothyroid ligament. It is variously described as being divided into the thyroarytenoid and vocalis muscle (or the thyromuscularis and the thyrovocalis), depending on the source. The thyroarytenoid muscle pulls the arytenoid cartilages forward toward the thyroid when it contracts, thereby loosening (relaxing and shortening) the vocal ligament (see below).
The fibres of the thyroarytenoid pass backward and lateralward, and are inserted into the base and anterior surface of the arytenoid cartilage. A considerable number of the fibres of the thyroarytenoid are prolonged into the aryepiglottic fold, where some of them become lost, while others are continued to the margin of the epiglottis. These fibres are called the thyreoepiglotticus or thyroepiglottic, and are sometimes described as a separate muscle. A few fibres extend along the wall of the ventricle from the lateral wall of the arytenoid cartilage to the side of the epiglottis and constitute the ventricularis muscle.
The lower and deeper fibres - the fine and most medial fibres - of the thyroarytenoid muscle can be differentiated as a triangular band originating from the depression between the two laminae of the thyroid cartilage and inserted into the vocal process of the arytenoid cartilages as well as portions of the vocal ligament, and into the adjacent portion of its anterior surface. This band is termed the vocalis or vocalis muscle, which lies parallel with the vocal ligament to which it is adherent (attached).
The vocalis muscle, as the name implies, is an important muscle for speech (and thus singing). The main function or action of the vocalis muscle is to adjust or alter the tension of small segments of the vocal folds in order to vary tonal qualities and pitches of the voice. It is a sphincter of vestibule that tightens the front part of the ligament near to the thyroid cartilage, thus narrowing the laryngeal inlet. It also supports the wall of the ventricle and its appendix. The vocalis muscle is innervated (supplied) by the recurrent laryngeal nerve.
The vocal ligaments, or inferior thyroarytenoid (thyroartenoideus internus), are two strong bands enclosed within the vocal folds. Each ligament consists of a band of yellow elastic tissue, attached in front to the angle of the thyroid cartilage, and behind to the vocal process of the arytenoid. They are constructed from epithelium (a tissue composed of cells that line the cavities and surfaces of structures throughout the body), but they have a few muscle fibres in them, namely the vocalis muscle. Owing to the connection of the deeper portion of the thyroarytenoid with the vocal fold, this part, if acting separately, is supposed to modify the fold's elasticity and tension, while the lateral portion rotates the arytenoid cartilage inward, and thus narrows the rima glottidis by bringing the two vocal folds together.
Various parts of the larynx are closed by connective tissue membranes, which include the cricothyroid membrane, the thyrohyoid membrane and the quadrangular membrane.
The cricothyroid membrane (or conus elasticus) extends from the upper margin of the cricoid cartilage and attaches to the back of the thyroid cartilage anteriorly and the arytenoid cartilage posteriorly. Its upper free margin is the vocal ligament (true vocal fold).
The thyrohyoid membrane is a tough, fibro-elastic ligament (or membrane) that connects the thyroid cartilage with the hyoid bone. It extends from the superior margin (upper border) of the thyroid cartilage below and the upper margin of the posterior surface of the body and greater cornua of the hyoid bone above. Essentially, it fills the gap between the hyoid bone and the thyroid cartilage. It is pierced by the internal laryngeal nerve and superior laryngeal artery.
The quadrangular membrane is free at the top and bottom but attached posteriorly to the arytenoid cartilage and anteriorly to the side of the epiglottis. The lower free margin forms the vestibular fold (false vocal fold).
EXTRINSIC MUSCLES OF THE LARYNX
The extrinsic muscles are larger muscles, located outside the larynx, that position and support the larynx. They may move the cartilages, which in turn, stretch or compress the vocal folds.
The thyrohyoid muscle is a small, quadrilateral muscle (belonging to the infrahyoid muscles group) that appears like an upward continuation of the sternothyroid muscle (next paragraph). It originates at the oblique line on the lamina of the thyroid cartilage and inserts into the inferior (lower) border of body and greater cornu (horn) of the hyoid bone. It depresses the hyoid and elevates the larynx.
The sternothyroid muscle is an infrahyoid muscle that originates from the posterior surface of the manubrium sterni (or episternum) and the first and sometimes second costal cartilages (the elastic cartilages that connect the sternum - breastbone - and the ends of the ribs, and allow the chest to move during respiration), with insertion into the oblique line of the lamina of the thyroid cartilage. (The manubrium sterni is the broad, upper part of the sternum that articulates with the clavicle - collar bone - and the first two ribs.) This muscle is shorter and wider than the sternohyoid muscle (paragraph below), beneath which it is situated. Its nerve supply comes from the upper cervical nerve through the cervical ansa. The sternothyroid muscle depresses the larynx and the thyroid cartilage for mastication (chewing) and swallowing.
The sternohyoid muscle is a thin, narrow muscle that arises from the posterior border of the medial end of the clavicle, the posterior sternoclavicular ligament, and the upper and posterior part of the manubrium sterni. Passing upward and medially, it is inserted by short tendinous fibres into the lower border of the body of the hyoid bone. The sternohyoid muscle attaches the hyoid bone to the sternum. It is one of the paired strap muscles of the infrahyoid muscles group, and it serves to depress the hyoid bone.
Pharyngeal constrictors are muscles that serve to constrict the pharynx. When the bolus of food (a ball of chewed food matter mixed with saliva) reaches the pharynx, the elevator muscles relax, allowing the pharynx to descend. The constrictors then contract upon the bolus, and convey it downward into the esophagus (the muscular tube through which food passes from the pharynx to the stomach). The pharyngeal constrictors include the superior pharyngeal constrictor muscle, the middle pharyngeal constrictor muscle (which arises from the whole length of the upper border of the greater cornu of the hyoid bone), and the inferior constrictor muscle.
The inferior pharyngeal constrictor is the thickest of the three pharyngeal constrictors. It arises from the thyroid cartilages (from the oblique line on the side of the lamina from the surface behind this, nearly as far as the posterior border, and from the inferior cornu) and the sides of the cricoid cartilage (in the interval between the cricothyroid muscle in front and the articular facet of the inferior cornu of the thyroid cartilage behind). The first (and more superior) part arising from the thyroid cartilage is called the thyropharyngeal part, and the second part arising from the cricoid cartilage is called the cricopharyngeal part. From these origins, the fibres spread backward and medialward to be inserted with the muscle of the opposite side into the fibrous pharyngeal raphe - a continuous ridge of tissue that serves as the origin and insertion for several of the pharyngeal constrictors - in the posterior median line of the pharynx. The fibres then diverge from their origin, with the lower fibres descending beneath the inferior constrictor, the middle fibres passing transversely, and the upper fibres ascending and overlapping the superior constrictor. The inferior fibres are horizontal and continuous with the circular fibres of the esophagus. The rest of the fibres ascend, increasing in obliquity, and overlap the middle constrictor from the lesser cornu and from the stylohyoid ligament (see below for definition).
The pharyngeal constrictors are all innervated by branches from the pharyngeal plexus (a network of nerve fibres innervating most of the palate, larynx and pharynx) and by neuronal branches from the recurrent (inferior) laryngeal nerve (a branch of the vagus nerve - tenth cranial nerve - that supplies motor function and sensation to the larynx).
Other extrinsic muscles associated with the larynx are the digastric, stylohyoid, mylohyoid, geniohyoid and hyoglossus muscles. These supplemental muscles are known as the laryngeal elevators (or the suprahyoid muscles) because they raise the larynx in the neck or support it. Some of these muscles are visible in images of the tongue, as they are also extrinsic muscles of the tongue.
The digastric is a small muscle located under the jaw and extending, in a curved form, from the mastoid process (the smooth, pyramidal or cone-shaped bone projections at the base of the skull on each side of the head just below and behind the ears) to the symphysis menti (the midline symphysis between the two halves of the mandible, or jaw) that acts to elevate the hyoid bone when it contracts. It consists of two fleshy bellies united by an intermediate rounded tendon. If the hyoid is being held in place (by the infrahyoid muscles), it will tend to depress the mandible and thus open the mouth.
The stylohyoid is a slender muscle lying anterior and superior to the posterior belly of the digastric muscle. It arises from the posterior and lateral surface of the styloid process of the temporal bone (a slender, pointed piece of bone located just below the ear that projects down and forward from the inferior surface of the temporal bone, and serves as an anchor point for several muscles associated with the tongue and larynx), near the base. Passing inferiorly and anteriorly, it is inserted into the body of the hyoid bone, at its junction with the greater cornu, and just superior the omohyoid muscle (an infrahyoid muscle located at the front of the neck, arising from the scapula and inserted into the body of the hyoid bone, that consists of inferior and superior bellies separated by an intermediate tendon, and acts to depress the hyoid bone during chewing and swallowing).
The mylohyoid is a flat and triangular muscle situated immediately above the anterior belly of the digastric muscle, and running from the mandible (lower jaw) to the hyoid bone, forming the floor of the oral cavity.
The geniohyoid is a narrow muscle situated superior to the medial border of the mylohyoid muscle, and is involved in driving food from the mouth into the pharynx and in depressing the mandible.
The hyoglossus is a thin and quadrilateral muscle that arises from the side of the body and from the whole length of the greater cornu of the hyoid bone, and passes almost vertically upward to enter the side of the tongue, between the styloglossus (a muscle with origin from the lower end of the styloid process, with insertion into the side and undersurface of the tongue, with nerve supply from the hypoglossal nerve, and whose action retracts the tongue) and longitudinalis inferior (a narrow band situated on the under surface of the tongue between the genioglossus and the hyoglossus). It depresses and retracts the tongue, making its dorsum (upper side) more convex. It is important in singing.
MUCOSAL LINING OF THE LARYNX
The vocal apparatus consists of two pairs of mucosal folds: the vestibular folds ('false vocal cords') and the true vocal folds.
The vestibular folds are located above both sides of the glottis (the hole and the ligament itself). They are covered by respiratory epithelium, and do not contain muscle. They are created by the mucosa passing over the vestibular ligament. They vibrate somewhat during phonation and especially during vibrato singing. Although they do play a role in resonance, these false folds, unlike the true vocal folds, are not actually responsible for sound production. The false vocal folds also work with the epiglottis to create a seal so that nothing goes down the trachea (windpipe) during swallowing.
'Vocal fold' is the current term for 'vocal cord'. (Most teachers and singers use these two terms interchangeably.) The change in terminology came about as the anatomy of the larynx, including the structure and function of the folds, came to be better understood by the scientific world. The folds are not a band of string suspended in the air that vibrates when it is plucked or struck, as the word 'cord' suggests. Instead, they are part of a muscle on the side of the larynx that is covered with special tissues that can vibrate at a high speed. (Only its outer covering actually vibrates.) A vocal fold resembles a lip of tissue much more than a cord, and the term 'fold' is, therefore, more accurate and preferable.
The true vocal folds are a pair of pliable shelves of tissue that stretch horizontally across the top of the larynx. They may also be described as twin infoldings covered on the surface by laryngeal mucous membrane (made up of elastic and fatty tissue, or stratified squamous epithelium), which is supported deeper down underneath by the innermost fibres of the thyroarytenoid muscle. They are flat, triangular bands, and are pearly white in colour. Unlike the false vocal folds, the true vocal folds do contain skeletal muscle. In most males, the vocal folds are longer and thicker and have more mass, producing a deeper pitch.
The folds are attached at the back to the vocal process of the arytenoid cartilages and to the thyroid cartilage at the front. They are enclosed within the thyroid cartilage, which is the hard structure that forms the mass in the neck known as the Adam's apple. Their outer edges are attached to muscle in the larynx and do not move or vibrate, while their inner edges, or margins, are free to vibrate.
Most of the muscles that act to abduct (open) or adduct (close) the vocal folds attach to the muscular process of the arytenoid cartilages. There is only one muscle that has an abductor action on the vocal folds - the posterior cricoarytenoid muscle - although there are several that act to adduct the folds. Abduction of the vocal folds may be accomplished either by externally rotating the arytenoid cartilages on a pivot located at their base or by sliding the two arytenoid cartilages apart slightly. Vocal fold length and tension can be controlled by rocking the thyroid cartilage forward and backward on the cricoid cartilage (either directly by contracting the cricothyroids or indirectly by changing the vertical position of the larynx), by manipulating the tension of the muscles within the vocal folds, and by moving the arytenoids forward or backward.
The vocal folds have a three-layer construction consisting of a cover called the epithelium or mucosa - (a tissue composed of cells that line the cavities and surfaces of structures throughout the body), a vocal ligament, and muscle fibre, which can shorten and bulge the folds by tightening the front part of the ligament near the thyroid cartilage. These three layers are also referred to as the superficial, intermediate and deep layers.
The cover of the folds is composed of the epithelium (mucosa), basal lamina (or basement membrane zone), and the superficial layer of the lamina propria. The soft, gel-like composition of the cover is important for creating the mucosal wave. The transition is composed of the intermediate and deep layers of the lamina propria. The body of the vocal fold is composed of the thyroarytenoid (vocalis) muscle. This layered structure of tissues is very important for vibration of the true vocal folds.
The epithelium, (the surface 'skin' of the larynx, which is continuous with the lining of the mouth, pharynx and with the trachea below the larynx), has been described as a thin shell, the purpose of which is to maintain the shape of the vocal fold. This epithelium is between five and twenty-five cells thick, with the most superficial layer consisting of one to three cells that are lost to abrasion of the vocal folds during the closed phase of vibration (the part of the vibratory cycle when the folds are together during phonation). The free edge of the vibratory portion of the vocal fold, the anterior glottis, is covered with stratified squamous epithelium, an epithelium characterised by its most superficial layer consisting of flat, scale-like cells called squamous cell. The posterior glottis is covered with pseudostratified ciliated epithelium, an epitheleum containing simple columnar epithelial cells whose nuclei appear at different heights, and also possessing fine hair-like extensions called cilia that waft unwanted particles out of the body. On the surfaces of the epithelial cells are microridges and microvilli, which help to spread and retain a mucuous coat on the epithelium. Lubrication of the vocal folds through adequate hydration is essential for normal phonation to avoid excessive abrasion. (Surgery of the vocal folds can disturb this layer with scar tissue, which can result in the inability of the epithelium to retain an adequate mucous coat, which will in turn impact lubrication of the vocal folds.)
The basal lamina, or basement membrane zone, is transitional tissue composed of two zones: the lamina lucida and lamina densa. The lamina lucida appears as a low density, clear zone medial to the epithelial basal cells. The lamina densa has a greater density of filaments and is adjacent to the lamina propria. The basal lamina mainly provides physical support to the epithelim through anchoring fibres, and is essential for repair of the epithelium.
The lamina propria has three distinct layers, each with a different consistency: the superficial layer, which has a jelly-like substance and is close to the surface, the intermediate layer, which is made up of an elastic, fibrous substance, and the deep layer, which is a thread-like collagenous fibre layer.
The superficial layer of the lamina propria consists of loose fibrous components and extracellular matrices - networks of non-living tissue (containing proteins, minerals, and certain carbohydrates) that provide support to cells, performing specific functions, depending on the types of cells that they are associated with - that can be compared to soft gelatin. This layer is also known as Reinke's space but it is not a space at all, although it is a potential space, (which would indicate a problem). The superficial layer of the lamina propria is a structure that vibrates a great deal during phonation, and the viscoelasticity needed to support this vibratory function depends mostly on these extracellular matrices. The primary extracellular matrices of the vocal fold cover are reticular, collagenous and elastic fibres, as well as glycoprotein and glycosaminoglycan. These fibres serve as scaffolds for structural maintenance, providing tensile (tension) strength and resilience so that the vocal folds may vibrate freely but still retain their shape.
The intermediate layer of the lamina propria is primarily made up of elastic fibres while the deep layer of the lamina propria is primarily made up of collagenous fibres. These fibres run roughly parallel to the vocal fold edge, and these two layers of the lamina propria comprise the vocal ligament. This transition layer is primarily structural, giving the vocal fold support as well as providing adhesion between the mucosa (cover), and the body (the thyroarytenoid or vocalis muscle).
FUNCTION OF THE LARYNX
Sound is generated in the larynx. Pitch and volume (loudness) are also manipulated at the laryngeal level.
During inhalation, the vocal folds spread apart in order to allow air into the lungs. (The muscles attached to the arytenoid cartilages control the degree of opening.) After inhalation, and just prior to speaking or singing, the folds are brought close together - they are approximated or closed - by adducting the arytenoid cartilages, which causes air pressure to build up beneath them. This pressure beneath the folds is refered to as subglottic (or subglottal) pressure.
This increased subglottic pressure causes the vocal folds to be pushed apart, with the inferior part of each fold leading the superior part. Air pushes through the very small space between them, the glottis, which then causes the covering of the vocal folds, known as the mucosa, to oscillate or vibrate. The vibration of the vocal folds modulates (regulates) the flow of air being expelled from the lungs, chopping up the steady stream of air into little puffs, thus generating sound. Under the correct conditions, this oscillation pattern will sustain itself.
The basic sound of the voice occurs by means of a phenomenon known as the venturi effect. As air passes through a constriction (or venturi), it speeds up and creates a suction in its wake. This suction draws in the pliable mucosa from each vocal fold, which meet in the midline, only to be pushed aside by more air escaping from the lungs. This cycle creates a repeating undulation known as the mucosal wave.
The regularity of the mucosal wave is essential to the production of good voice. A number of factors can influence the formation and maintenance of the mucosal wave. The two main factors involve vocal fold closure and the integrity of the superficial layer of the lamina propria. Inability of the vocal folds to close sufficiently, as in some cases of vocal fold paralysis (when one or both vocal folds are paralyzed), may make it impossible to create the venturi effect, which underlies mucosal vibration. Tethered or stiff mucosa resulting from a change in the lamina propria, as in a vocal fold scar, will not vibrate well or at all, regardless of the vocal fold closure. Sometimes, a large mass like a cyst, polyp or nodule (vocal node) blocks both the vocal folds from closing and the mucosa from vibrating. Irregularity of mucosal vibration also results in problems like hoarseness.
The frequency of the mucosal wave determines the pitch of the voice. Fine manipulation of the larynx is used to generate a source sound with a particular fundamental frequency, or pitch. Pitch is altered (caused to either rise or fall) by the changing tenseness and length of the vocal folds, which can be controlled by rocking the thyroid cartilage forward and backward on the cricoid cartilage, (a mechanism known as the 'laryngeal tilt'), and by manipulating the tension of the muscles within the vocal folds. (Increasing vocal fold tension by lengthening the folds and making them more taut produces a higher pitch.) To maintain consistent phonation and healthy vocal fold function, tension must be altered symmetrically (by both folds simultaneously and equally). These changes in pitch occur rapidly and precisely many times during speaking tasks as the speaker inflects his or her voice. Intentional and repeated patterns of pitch give rise to melody.
The volume of sound is principally a result of the pressure of the air that is blown past the vocal folds. A more forceful expulsion of air from the lungs raises this pressure and creates a louder sound. The vocal folds must increase tension to maintain the near-closure that is needed for the venturi effect. If they do not, the increased air pressure will simply blow them aside and interrupt vibration, causing a cessation in sound production. This tensing of the vocal folds usually happens instinctively, without conscious effort. However, people with vocal fold paralysis or other types of vocal fold pathologies and/or weakness are often unable to do this, and frequently complain of an inability to increase the volume of their voices.
This initial source sound generated in the larynx is then altered as it travels through the vocal tract, configured differently based on the position of the tongue, lips, mouth, and pharynx. The process of altering a source sound as it passes through the filter of the vocal tract, is known as articulation, which creates the many different vowel and consonant sounds of the world's languages.
HOW PUBERTY AND AGING AFFECT THE SINGING VOICE
The age and physical development of a singer significantly impact the kind and quality of sound that is produced by the larynx, as well as how vocal instruction must be approached. Every age group has its own unique needs, as I will explain in more depth in this section, and it is important for vocal teachers, singers and parents to take into consideration these changes that occur to the voice over time. Understanding the development of the vocal instrument will ensure that expectations remain more realistic, frustration is minimized, success, (even if redefined with every stage of development), is achieved, and optimal vocal health is maintained.
In infants, the lamina propria is composed of only one layer, and there is no vocal ligament. At about four years of age, the vocal ligament begins to be present in children. Between the ages of six and twelve, two layers appear in the lamina propria. By the conclusion of adolescence, the mature three-layered lamina propria is present.
This presence or absence of tissue layers influences a difference in the number of vocal formants between the adult and pediatric populations because vocal fold vibration is a foundation for formants. For example, the voice of an adult female is three tones lower than that of a child, and has five to twelve formants. The child's voice has only three to six vocal formants.
At birth, the length of the vocal fold is approximately six to eight millimetres. It grows to its adult length of eight to sixteen millimetres during adolescence.
The infant vocal fold is half membranous (or anterior glottis), and half cartilaginous (or posterior glottis), whereas the adult fold is approximately three-fifths membranous and two-fifths cartilaginous.
During puberty, which typically occurs between the ages of twelve and seventeen, both the voices of males and those of females undergo change. Voice change is controlled mainly by sex hormones, although the physical growth (and thus size) of the laryngeal structures does play a role, as well. The different hormones present between males and females create different kinds of changes.
Testosterone is the primary and most well-known androgen or androgenic hormone. In males, androgens are essential to male sexuality, as they stimulate or control the development and maintenance of male characteristics, which includes the activity of the accessory male sex organs and development of male secondary sex characteristics (such as facial hair). Androgens are the most important hormones responsible for the passage of the boy-child voice to man voice, and the change is irreversible. When secreted by the testes of males, testosterone will cause changes in the cartilages and musculature of the larynx for males during puberty. The thyroid prominence or laryngeal prominence (Adam's apple) appears, the vocal folds lengthen and become rounded, and the epithelium thickens with the formation of three distinct layers in the lamina propria. In muscles, they cause a hypertrophy (enlargement) of striated muscles with a reduction in the fat cells in skeletal muscles, and a reduction in the whole body fatty mass, leading to more muscle bulk.
Androgens are also the original anabolic steroids and the precursor of all estrogens, the female sex hormones. In women, androgens are secreted principally by the adrenal cortex and the ovaries, and can have irreversible masculinizing effects if present in excessively high concentrations.
For women, the actions of estrogens and progesterone produce changes in the extravascular spaces by increasing capillary permeability, which allows the passage of intracapillary fluids to the interstitial space as well as modification of glandular secretions.
Estrogens have a hypertrophic (enlarging) and proliferative (increasing or multiplying by cell division) effect on mucosa by reducing the desquamating effect on the superficial layers.
Progesterone has an anti-proliferative (decreasing) effect on mucosa and accelerates desquamation. It causes a menstrual-like cycle in the vocal fold epithelium and a drying out of the mucosa with a reduction in secretions of the glandular epithelium. Progesterone has a diuretic (drying out by inhibiting the body's ability to re-absorb fluid, which leads to a retention of water in the urine and mild dehydration) effect and decreases capillary permeability, thus trapping the extracellular fluid out of the capillaries and causing tissue congestion. This cyclical hormonal change causing a drying out of the vocal instrument explains why some women notice subtle changes in their voice quality during their menstrual cycles. Some professional female opera singers even schedule performances around their cycles so that they can offer their audiences the best performance possible and so that they don't risk damaging their voices when there is insufficient moisture or lubrication for the folds to function optimally.
The thyroid hormones also affect dynamic function of the vocal folds. (Hashimoto's Thyroiditis, for example, affects the fluid balance in the vocal folds).
In females during puberty, the thyroarytenoid muscle thickens slightly, but remains very supple and narrow. The squamous mucosa, (an epithelium characterised by its most superficial layer consisting of flat, scale-like cells called squamous cell), also differentiates into three distinct layers (the lamina propria) on the free edge of the vocal folds. The subglottic (below the glottis) and supraglottic (above the glottis) glandular mucosa become dependent on estrogens and progesterone hormones.
As humans age, there is a steady increase in the elastin (a yellow scleroprotein, the essential constituent of the elastic connective tissue) content of the lamina propria, resulting in a decrease in the ability of the lamina propria to expand caused by cross-branching of the elastin fibres. Among other things, this leads to the mature voice being better suited to the rigors of opera.
In old age, there is a thinning in the superficial layer of the lamina propria. In aging, the vocal fold undergoes considerable sex-specific changes. In the female larynx, the vocal fold cover thickens. The superficial layer of the lamina propria loses density as it becomes more edematous (inflammed or marked by edema). The intermediate layer of the lamina propria tends to atrophy only in men. The deep layer of the lamina propria of the male vocal fold thickens because of increased collagen deposits. The vocalis muscle atrophies in both men and women. However, the majority of elderly patients with voice disorders have diseased processes associated with aging rather than physiologic aging alone.