Nursing Care Plan for Seizure
Introduction:
Seizures are episodes of abnormal electrical activity in the brain that can result in various physical and psychological manifestations. As a nurse, your role is crucial in providing safe and effective care during seizures and promoting the overall well-being of individuals with seizure disorders. This nursing care plan aims to outline evidence-based interventions to assess, manage, and support patients experiencing seizures.
Patient Information:
- Name: [Patient’s Name]
- Age: [Patient’s Age]
- Gender: [Patient’s Gender]
- Medical History: [Brief summary of patient’s medical history]
- Type of Seizure: [Identify the specific type of seizure experienced by the patient]
- Triggers or Provoking Factors: [Identify any known triggers or factors that may induce seizures]
- Medical Diagnosis: Seizure Disorder
- Date of Admission: [Date of Admission]
- Date of Care Plan: [Date of Care Plan]
Assessment:
Subjective Data:
- The patient may report a history of seizures, describing the frequency, duration, and triggers if known.
- Patients may express concerns about the impact of seizures on daily activities and quality of life.
Objective Data:
- Observations of seizure activity, noting the type of seizure (e.g., generalized tonic-clonic, absence, focal) and associated symptoms.
- A post-ictal state characterized by confusion, drowsiness, and fatigue.
- Medication history, including antiepileptic drugs (AEDs) and their effectiveness.
Nursing Diagnosis for Seizure:
- Risk for Injury related to potential falls or trauma during seizures.
- Ineffective Coping related to the emotional impact and lifestyle limitations associated with seizures.
- Impaired Verbal Communication related to altered consciousness or post-seizure confusion.
- Deficient Knowledge regarding seizure management, triggers, and safety precautions.
- Risk for Injury related to seizure activity as evidenced by observed seizures and associated risks (e.g., falls, aspiration).
- Deficient Knowledge related to seizure management as evidenced by the patient’s request for information and concerns about seizure triggers and prevention.
- Impaired Quality of Life-related to the impact of seizures on daily activities and emotional well-being as evidenced by the patient’s expression of concerns and limitations.
Nursing Interventions of Seizure:
Risk for Injury:
- Assess the patient’s seizure frequency, duration, and triggers to identify patterns and potential risks.
- Ensure a safe environment by removing any hazardous objects or furniture that may cause injury during seizures.
- Educate the patient and caregivers about seizure precautions, including placing soft padding on the floor, using helmets if necessary, and avoiding activities with a high risk of injury.
- Collaborate with the healthcare team to consider the use of antiepileptic medications or other interventions to reduce seizure frequency and severity.
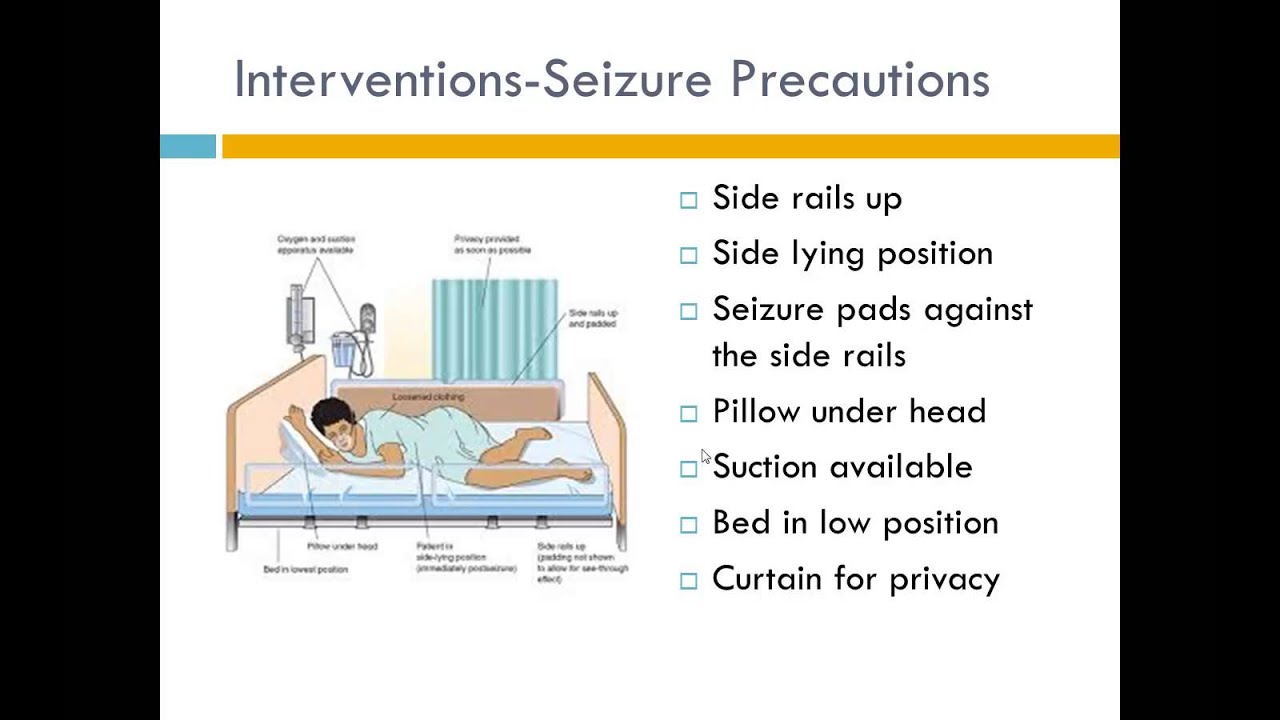
- Ensure a safe environment by removing potential hazards and padding sharp corners or edges.
- During a seizure, protect the patient from injury by guiding them to the floor if necessary, clearing the area of objects that may cause harm, and cushioning their head.
- Position the patient on their side to prevent aspiration and maintain a patent airway.
- Administer prescribed antiepileptic medications as ordered to reduce the frequency and severity of seizures.
- Collaborate with the healthcare team to explore additional interventions, such as assistive devices or seizure response plans, to further reduce the risk of injury.
Deficient Knowledge:
- Assess the patient’s understanding of seizures and seizure management.
- Provide education about seizure triggers, such as lack of sleep, stress, or certain stimuli, and strategies to avoid or manage them.
- Teach the patient and their family or caregivers about appropriate first aid measures during a seizure, including maintaining a safe environment and timing the seizure duration.
- Educate the patient about the importance of medication adherence, the potential side effects of AEDs, and the need for regular follow-up appointments with their healthcare provider.
- Refer the patient to support groups or educational resources for additional information and emotional support.
Impaired Quality of Life:
- Assess the patient’s perception of the impact of seizures on their daily activities and emotional well-being.
- Encourage the patient to express their concerns and frustrations related to seizure management.
- Assist the patient in identifying strategies to maintain or improve their quality of life, such as stress management techniques, maintaining a regular sleep schedule, and engaging in enjoyable activities.
- Collaborate with the healthcare team to adjust medication regimens or explore alternative therapies if necessary to optimize seizure control and minimize side effects.
- Provide emotional support and refer the patient to appropriate mental health resources, such as counseling or therapy, to address any psychological or emotional challenges associated with the seizure disorder.
Ineffective Coping:
- Assess the patient’s emotional well-being and the impact of seizures on their quality of life and relationships.
- Provide emotional support and a non-judgmental environment for the patient to express their feelings and concerns.
- Encourage the patient to participate in support groups or counseling to cope with the emotional and psychological challenges associated with seizures.
- Educate the patient and caregivers about stress management techniques, relaxation exercises, and lifestyle modifications that may help reduce seizure triggers.
Impaired Verbal Communication:
- During and after seizures, provide a calm and reassuring presence to the patient.
- Document the duration and characteristics of the seizure, as well as any post-seizure confusion or disorientation.
- Allow time for the patient to recover and regain verbal communication skills.
- Utilize alternative communication methods, such as gestures, writing, or using communication boards, if verbal communication is temporarily impaired.
Deficient Knowledge:
- Assess the patient’s understanding of seizure management, triggers, and safety precautions.
- Provide education about the patient’s specific type of seizure, including signs and symptoms, potential triggers, and appropriate responses.
- Teach the patient and caregivers how to administer first aid during seizures, including protecting the patient from injury, turning them on their side, and ensuring a patent airway.
- Discuss the importance of medication adherence and follow-up appointments with the healthcare provider.
Evaluation and Expected Outcomes:
- Prevention of injuries during seizures through the implementation of safety measures.
- Improved coping skills and emotional well-being in managing the lifestyle limitations associated with seizures.
- Effective communication and resolution of post-seizure confusion or disorientation.
- Enhanced knowledge and understanding of seizure management, triggers, and safety precautions.
- The patient experiences a reduced risk of injury during seizure episodes.
- The patient demonstrates an improved understanding of seizure management, including triggers, first aid measures, and medication adherence.
- The patient reports an improved quality of life, with a reduction in seizure-related limitations and emotional distress.
- The patient actively engages in self-management strategies and seeks appropriate support when needed.
Documentation:
Regularly document the patient’s seizure activity, interventions provided, and the outcomes achieved. Collaborate with the interdisciplinary healthcare team to review and update the care plan based on the patient’s response to treatment and evolving needs.
Note: This nursing care plan is a general guideline and should be individualized based on the patient’s specific needs, seizure type, and healthcare provider’s recommendations.
